What is a Coronary Artery stent? A coronary stent is stainless tube with slots. It is mounted on a balloon catheter in a “crimped” or collapsed state. When the balloon of is inflated, the stent expands or opens up and pushes itself against the inner wall of the coronary artery. This holds the artery open when the balloon is deflated and removed. Coronary artery stents were designed to overcome some of the short comings of angioplasty. Angioplasty is a technique that is used to dilate an area of arterial blockage with the help of a catheter with an inflatable, small, sausage-shaped balloon at its tip. Although introduced over two decades ago, angioplasty continues to be the most frequently employed procedure in the cardiac cath lab (either by its self, or in conjunction with other procedures such as coronary stenting).
However, coronary angioplasty has two shortcomings. Firstly, the opening created by the procedure is not very smooth because the balloon does not evenly expand all areas that have different degrees of hardness (atheroma is soft, plaques are hard and mixture of the two have a medium and uneven degree of hardness). This produces a channel with an irregular shape and a rough surface that is covered with superficial or deep cracks. The irregular surface and the cracks on the inner lining of the artery increases the risk of complete arterial blockage in a very small number of patients. The picture on the left (below) shows a blockage prior to angioplasty, while the picture in the middle demonstrates the artists rendition of the angioplasty results.
Secondly, some of the compressed material tends to “spring back” to some degree. This is known as “recoil.” Recoil causes the channel to become smaller shortly after being enlarged by balloon expansion. Moreover, the material within the expanded channel starts to multiply after the channel is expanded. This causes a gradual build-up of material. In 30-60% of cases, the build-up of material can be large enough to cause the blockage to return to its original (or worse) severity. This occurs over a 6 week to 6 month duration of time and is known as restenosis.

The picture on the left (above) shows a cross-section of a coronary artery at the level of a blockage or stenosis. The diagram on the extreme right shows an increased opening after the blockage was treated with a coronary stent. A stent is a metal “mesh” that is mounted on an angioplasty balloon. When the balloon is inflated, it expands the stent and opens up the diseased segment into a rounder, bigger and smoother opening (compared to angioplasty, which is shown in the middle picture as having a more “frayed” appearance), Stents induce a more predictable and satisfactory result, reduces the risk of the artery abruptly closing off during the procedure and also decreases the chance of restenosis (recurrence of the blockage) by nearly 50% (from 30-50% in cases of angiopalsty, down to 15-25% in cases of stents).
Like angioplasty, coronary stents physically opens the channel of diseased arterial segments, relieves the recurrence of chest pain, increases the quality of life and reduces other complications of the disease. Since it is performed through a little needle hole in the groin (or sometimes the arm) it is much less invasive than surgery and can be treated with another needle or percutaneous procedure should the patient develop disease in the same, or another, artery in the future.
Prior to performing stenting, the location and type of blockage plus the shape and size the coronary arteries have to be defined. This helps the cardiologist decide whether it is appropriate to proceed with angioplasty or to consider other treatment options such angioplasty, atherectomy, medications or surgery. Cardiac catheterization (cath) is a specialized study of the heart during which a catheter or thin hollow flexible tube is inserted into the artery of the groin or arm. Under x-ray visualization, the tip of the catheter is guided to the heart. Pressures are measured and an x-ray angiogram (angio) or movie of the heart and blood vessels is obtained while an iodine- containing colorless “dye” or contrast material is injected into the artery through a catheter. The iodinated solution blocks the passage of x-rays and causes the coronary arteries to be visualized in the angios. In other words, coronary arteries are not ordinarily visible on x-ray film. However, they can be made temporarily seem by filling them with a contrast solution that blocks x-ray.
As discussed in the cardiac cath section, a sheath is introduced in the groin (or occasionally in the arm). Through this sheath, a long, flexible, soft plastic tube or guiding catheter is advanced and the tip positioned into the opening or mouth of the coronary artery. In the picture below, the catheter tip is positioned in the mouth of the left main coronary artery.
The tube measures 2 to 3 mm in diameter. The tip of the catheter is directed or controlled when the cardiologist gently advances and rotates the end of the catheter that sits outside the patient.
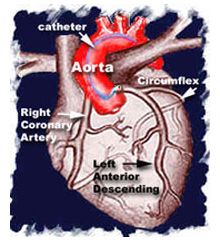
Once the catheter tip is seated within the opening of the coronary artery, x-ray movie pictures are recorded during the injection of contrast material or “dye.”
After evaluating the x-ray movie pictures, the cardiologist estimates the size of the coronary artery and selects the type of balloon catheter and guide wire that will be used during the case. Heparin (a “blood thinner” or medicine used to prevent the formation of clots is given. In most cases, coronary stenting is preceded by angioplasty. This is known as “pre-dilation.” It helps open up the blockage area, and makes it easier to deliver the stent.
The guide wire which is an extremely thin wire with a flexible tip is inserted into the catheter. The tip of the wire is then guided across the blockage and advanced beyond it. This wire now serves as a “guide” or rail over which the balloon catheter is passed. The tip of the stent balloon catheter is then positioned across the lesion. The balloon is situated on the tip of the catheter shaft and is inflated by connecting it to a special hand-held syringe pump. A mixture of saline and contrast material is used to inflate the balloon. The balloon catheter has metallic markers (at either side of the balloon). The unexpanded stent is mounted just inside these visible metallic markers that helps the cardiologist know the location of the otherwise poorly visible stent.
Inflation is initially carried out at a pressure of 1 – 2 times that of the atmosphere and then increased to 8 – 12 and sometimes as high as 20 atmospheres, depending upon the type of stent that is used. The handheld inflation syringe has markers that are used to determine the pressure. The balloon is kept inflated for 30 to 60 seconds and then deflated. The expanded stent is embedded into the wall of the diseased artery, holding it open. If not satisfied by the results, the cardiologist will further expand the stent using another balloon (frequently it is the same balloon catheter that was used for “pre-dilation.”.
The video on the left (above) shows a 95% blockage in the proximal portion of the left anterior descending coronary artery (arrow). The video to its right shows no remaining blockage after the patient was treated with a coronary artery stent.
The patient remains awake throughout the procedure and mild sedation is used to ensure relaxation and comfort. The deflated balloon and wire are withdrawn when the cardiologist is satisfied with the results.
The sheath is secured to the groin and the patient is sent to his or her room. The sheath is removed when the effect of Heparin wears off. This is determined by obtaining blood tests at specified intervals. Pressure is applied to the groin with a clamp. Once it is confirmed that there is no bleeding, a sandbag or ice bag is placed over the groin.
After approximately 6 hours, the patient is ambulated or allowed to walk with assistance and is usually discharged the following morning. A Band-Aid or small dressing is applied over the tiny needle hole. Slight bruising around the site is not uncommon.
In some labs, a sealant device is applied in the cath lab after removal of the sheath.
For a description of the equipment, preparation and experiences during the procedure, please review the cardiac cath section. It is not uncommon for patients to experience chest discomfort while the balloon is inflated. This usually resolves when the balloon is deflated. Patients who are uncomfortable can be given intravenous medication to alleviate this problem.
It can take anywhere from 30 minutes to an hour to perform the entire case. The duration is dependent upon the technical difficulty of the case and the number of balloon catheters that have to be employed.
In the hands of experienced cardiologists, and with availability of modern day technology, it is estimated that the risk of death is during a stent procedure is usually less than 1%, while the chance of requiring emergency bypass surgery is around 2% or less. It is a relatively safe procedure and is carried out all over the world. An “out patient” or an inpatient uncomplicated stent case usually require 23 hours or less of hospitalization after the procedure.
The risk of a other serious complication is estimated to be less than 4 and probably around 1 to 2 per thousand, and similar to that described for cardiac cath. The risk of a heart attack and bleeding that requires a blood transfusion is increased when compared to cardiac cath. However, the risks are relatively low and acceptable in most cases when one balances the potential benefit against the expected risk (risk-benefit ratio).
The aggravation of kidney function (particularly in diabetics and those with prior kidney disease) is higher than that expected with cardiac cath because of the larger amount of contrast material that is usually required. In such cases, the cardiologist takes extra precautions to prevent this possible complication.
The stent is completely covered by natural tissue in a matter of 4 – 6 weeks.and the risk of clot formation is nearly absent by that time. In very few cases (1 chance out of 200) a clot may form during the first two weeks after a stent procedure). Such patients develop symptoms of a heart attack. With prompt treatment, the majority of these stents can be reopened.
If coronary artery stenting is superior to angioplasty, why is it not used in every single case? Good question! If stents could be delivered to every lesion, and if it had the same good short and long term results in every case, it would be used in 100% cases of angioplasty. However, this is not the case. Stents are difficult to deliver across tight bends in blood vessels (particularly if they have a lot of calcium deposits in the wall) and are not usable in very small blood vessels. There are other types of technical considerations that also come into play. Today, it is estimated that stents are employed in nearly 50-75% of cases.
What special treatment is needed after a coronary stent procedure? Coronary artery stents are foreign metallic objects that are left inside the coronary artery. Special precautions have to be taken to prevent them from being covered with clot. Medications that make platelets less active has been found to be extremely effective in preventing clots. A combination of soluble aspirin (Bayer Aspirin* is an example) and Plavix* is very popular in the USA. (* = Trade Names of the manufacturers). The medications are started either before or during the procedure. Aspirin is continued indefinitely if the patient is not allergic to the medication and does not develop any problems with it. Plavix* is usually stopped in 4 – 6 weeks because the stent is usually completely covered by natural tissue during that period and the risk of clot formation is nearly absent by that time.
If patients are allergic to aspirin or Plavix(R) or are unable to take medication because of bleeding or other problems, the cardiologist may employ alternative medications (depending upon the problem) and even delay or avoid the use of a stent.
Drug eluting stents (DES) and late thrombosis or clot formation: Bare-metal or non-drug coated stents are usually fully coated by body tissue within a few weeks. Once this occurs the stent becomes more resistant to clots and Plavix* can usually be discontinued about 2 months after it is deployed or put in place.
In contrast, drug eluting stents (DES) do not become fully coated with normal tissue for 6 to 12 months, or even longer. Discontinuation of Plavix* prior to this time can result in clot formation and a heart attack. Thus, it is extremely important that patients with a stent (particularly DES) should not stop taking Plavix* until after seeking approval from their cardiologist.
The drug-coated stents are significantly more costly than non-coated stents. However, economic analysis performed independently by researchers have confirmed the cost-effectiveness of the drug-eluting coronary stent (DES). There been used actual hospital in-patient and out-patient cost data, beginning with the period of initial hospitalization and ending one year following stent implantation.
Been reported that, “Over the one-year follow-up period, patients who received the DES showed substantial reductions in the need for repeat treatments and re hospitalization, translating into substantial post-treatment healthcare savings,”. “During 12-month follow-up, for every 100 patients treated with the DES, there were 19 fewer revascularization procedures and 25 fewer hospital admissions than with the conventional stent.”
Insertion of the drug-eluting stent is similar to that of the conventional coronary stent.
 ROMANA
ROMANA